When patients consider lipedema reduction surgery, one of the most common questions Dr. Wright encounters is, “How much fat will be removed?” While this seems like a logical concern, the reality of lipedema surgery is far more complex than simple volume measurements. Understanding what actually comes out during liposuction (the lipoaspirate) can help set realistic expectations and explain why focusing solely on volume removed often leads to disappointment.
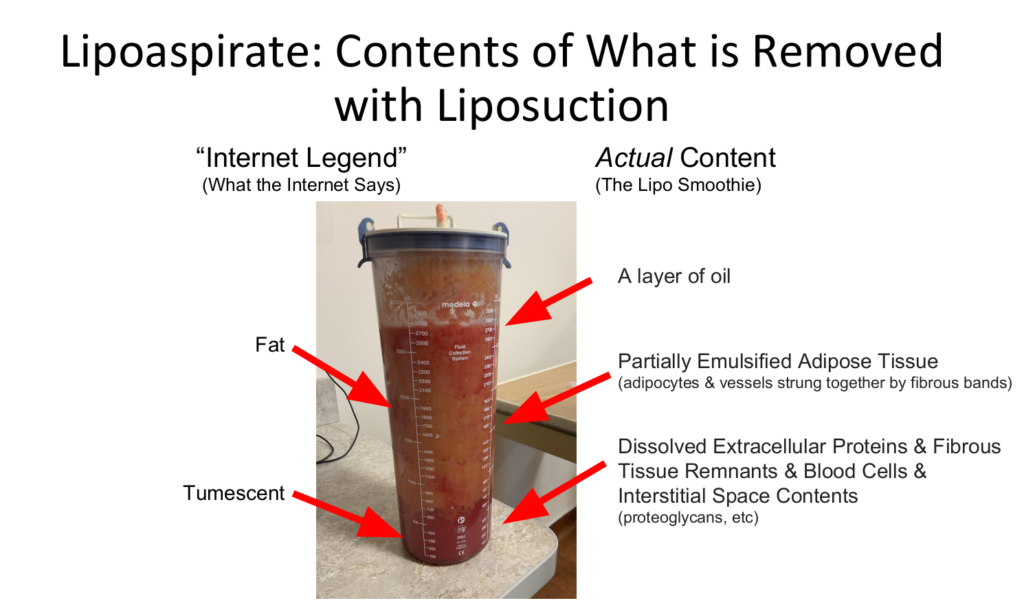
What Is Lipoaspirate? The “Lipo Smoothie” Explained
The material removed during lipedema liposuction is called lipoaspirate, sometimes colloquially referred to as “lipo smoothies” by surgeons due to its consistency and appearance. This complex mixture is far from pure fat tissue. Instead, it contains a sophisticated combination of cellular components, debris, and dissolved substances that vary significantly from patient to patient.
When Dr. Wright performs lipedema reduction surgery, he begins by infiltrating the treatment area with tumescent fluid, a sterile solution containing local anesthetic and other medications. This liquid is then combined with the semi-solid subcutaneous adipose tissue through mechanical agitation and suction, creating an emulsified mixture that can be safely removed from the body.
The composition of this aspirate depends on numerous factors that make volume predictions challenging and often misleading. The amount of tumescent fluid used, the timing between infiltration and suction, the specific body area being treated, and the surgeon’s experience all influence what ultimately comes out during the procedure.
The Unique Composition of Lipedema Tissue
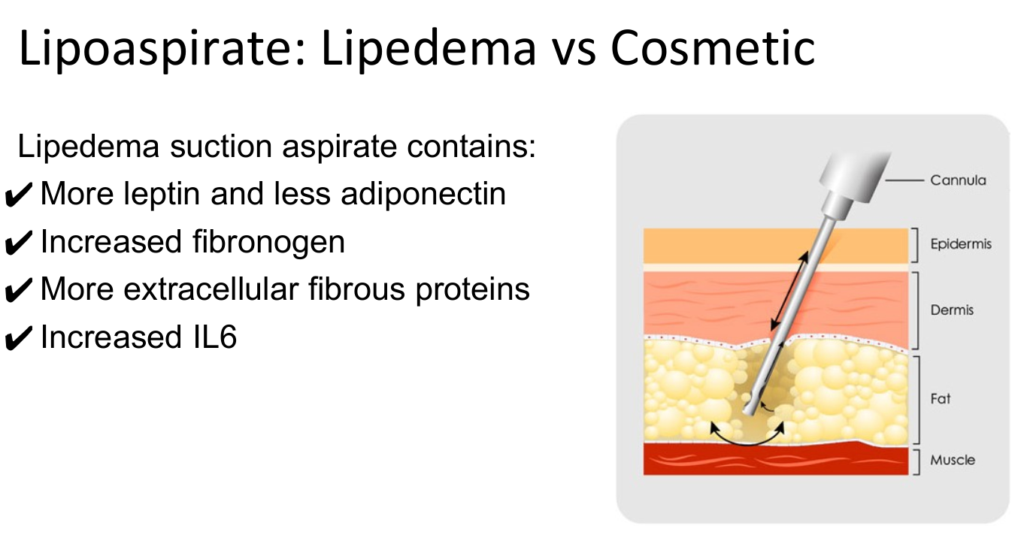
Research has revealed that lipedema tissue differs significantly from normal adipose tissue in both structure and biochemical composition. These differences help explain why traditional liposuction techniques require modification for lipedema patients and why volume alone is not an adequate measure of surgical success.
Biochemical Differences
Lipedema suction aspirates contain distinct molecular markers that set them apart from normal fat tissue:
Elevated Leptin Levels: Leptin, often called the “satiety hormone,” is found in much higher concentrations in lipedema tissue. This hormone normally signals fullness and helps regulate energy balance, but in lipedema patients, the tissue appears to have altered leptin signaling pathways.
Reduced Adiponectin: This beneficial hormone, which helps regulate glucose levels and fatty acid breakdown, is found in lower concentrations in lipedema aspirates. The imbalance between leptin and adiponectin may contribute to the metabolic dysfunction associated with lipedema.
Increased Inflammatory Markers: Higher levels of interleukin-6 (IL-6), a pro-inflammatory cytokine, are consistently found in lipedema tissue. This chronic inflammatory state helps explain the pain and tenderness characteristic of the condition.
Structural Differences
The physical composition of lipedema tissue also differs markedly from normal fat:
Enhanced Fibrous Content: Lipedema tissue contains significantly more fibrous proteins, including fibronectin and collagen. This increased fibrosis creates the nodular, uneven texture that patients feel and contributes to the tissue’s resistance to conservative treatments.
Increased Fibrinogen: Higher concentrations of this coagulation protein suggest altered blood clotting mechanisms within lipedema tissue, which may contribute to the easy bruising many patients experience.
Extracellular Matrix Changes: The supportive structure surrounding fat cells is dramatically altered in lipedema, creating a more rigid and fibrous environment that traps fluid and contributes to pain.
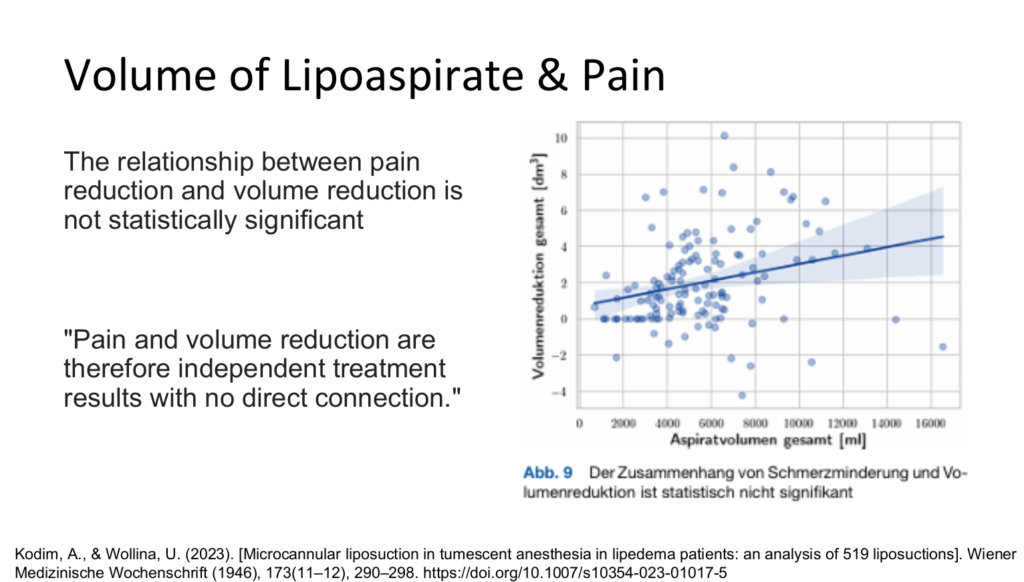
Why Volume Doesn’t Predict Pain Relief
One of the most important concepts for lipedema patients to understand is that the volume of tissue removed during surgery does not correlate with pain relief. This counterintuitive finding has profound implications for how we approach surgical planning and set patient expectations.
Dr. Wright emphasizes this principle because research consistently demonstrates that pain reduction and volume removal are independent treatment outcomes. A landmark study by Kodim and Wollina (2023) analyzing 519 lipedema liposuctions confirmed this finding, stating that “Pain and volume reduction are therefore independent treatment results with no direct connection.”
The Science Behind Pain Relief
Pain in lipedema appears to result from multiple mechanisms:
Pressure on Nerve Endings: The altered tissue structure and increased fibrosis create mechanical pressure on sensory nerves, leading to both spontaneous pain and tenderness to touch.
Inflammatory Processes: The chronic inflammation within lipedema tissue sensitizes pain receptors and creates an environment of persistent discomfort.
Vascular Changes: Altered blood flow and lymphatic drainage contribute to the sensation of heaviness and aching that patients describe.
Tissue Tension: The rigid, fibrotic nature of lipedema tissue creates internal tension that manifests as pain and discomfort.
When Dr. Wright performs lipedema reduction surgery, the goal is to address these underlying pain mechanisms rather than simply removing the maximum volume of tissue. Strategic removal of the most problematic tissue areas, combined with techniques that improve lymphatic drainage and reduce tissue tension, provides superior pain relief compared to aggressive volume-focused approaches.
The Dangers of Volume Obsession
Research has identified a concerning pattern among lipedema patients: those who focus excessively on the volume of fat to be removed before surgery are significantly more likely to be dissatisfied with their results. Studies show these patients are up to 17 times more likely to report disappointment with their surgical outcomes, even when the procedure successfully achieves its primary goals of pain reduction and improved function.
This dissatisfaction stems from unrealistic expectations about what liposuction can and cannot achieve in lipedema patients. Unlike cosmetic liposuction performed on healthy tissue, lipedema surgery must balance multiple competing priorities:
Safety Considerations
Lymphatic Preservation: Aggressive volume removal can damage the already compromised lymphatic system in lipedema patients, potentially worsening swelling and creating new complications.
Tissue Viability: Removing too much tissue can compromise blood supply to remaining areas, leading to poor healing and increased risk of complications.
Contour Irregularities: Excessive tissue removal often results in uneven contours and dimpling that can be more cosmetically problematic than the original condition.
Functional Goals
Pain Reduction: Strategic tissue removal targeting the most problematic areas often provides better pain relief than maximum volume extraction.
Mobility Improvement: Removing tissue that restricts movement and function takes precedence over achieving maximum volume reduction.
Long-term Stability: Conservative volume removal with attention to tissue health often provides more durable results than aggressive approaches.
Factors Influencing Aspirate Composition
Understanding the variables that affect lipoaspirate composition helps explain why no two lipedema surgeries are identical, even in the same patient:
Tumescent Fluid Variables
Infiltration Volume: The amount of tumescent solution used affects the final aspirate volume but doesn’t necessarily indicate more fat removal.
Timing: The interval between fluid infiltration and suction influences how much liquid remains in the final aspirate.
Composition: Different tumescent formulations can alter the physical and chemical properties of the aspirate.
Anatomical Factors
Body Region: Different areas of the body have varying tissue densities and fibrous content, affecting aspirate composition.
Disease Stage: Advanced lipedema with more fibrosis will produce aspirates with different characteristics than early-stage disease.
Previous Treatments: Areas previously treated with compression or other interventions may have altered tissue properties.
Surgical Technique Factors
Cannula Selection: Different cannula types and sizes affect tissue breakdown and aspirate consistency.
Suction Pressure: The vacuum level used influences what components are extracted versus left behind.
Surgeon Experience: Skilled surgeons can more effectively target problematic tissue while preserving healthy structures.
Dr. Wright’s Approach: Quality Over Quantity
Dr. Wright’s extensive experience with lipedema reduction surgery has reinforced the importance of prioritizing tissue quality and patient symptoms over volume metrics. His approach focuses on:
Comprehensive Assessment
Before surgery, Dr. Wright conducts thorough evaluations that go far beyond measurements and photos. He assesses pain patterns, functional limitations, and the impact on quality of life to develop individualized treatment plans that address each patient’s specific needs.
Strategic Planning
Rather than attempting maximum volume removal, surgical planning focuses on targeting the areas most responsible for pain and functional impairment. This selective approach often provides superior symptom relief with lower complication rates.
Realistic Expectation Setting
Dr. Wright ensures that patients understand the goals of lipedema surgery and the limitations of volume-based assessments. This education process helps prevent the disappointment that comes from unrealistic expectations about dramatic size reductions.
Multi-Modal Treatment
Recognizing that lipedema is a complex condition requiring comprehensive care, Dr. Wright integrates surgical interventions with conservative treatments, post-operative care protocols, and long-term management strategies.
Post-Operative Considerations
Understanding lipoaspirate composition also helps explain post-operative experiences that might otherwise be concerning:
Expected Changes
Swelling Patterns: The inflammatory nature of lipedema tissue can lead to prolonged swelling as the body processes cellular debris and inflammatory mediators.
Healing Timeline: The fibrous nature of lipedema tissue may result in longer healing times compared to cosmetic liposuction on healthy tissue.
Pain Evolution: As inflammation subsides and tissue remodels, pain relief may continue to improve for months after surgery.
Monitoring Progress
Rather than focusing on immediate volume changes, Dr. Wright monitors progress through functional assessments, pain scores, and quality of life measures. These metrics provide more meaningful insights into surgical success than simple measurements.
The Future of Lipedema Surgery
Advancing understanding of lipoaspirate composition is opening new avenues for improving lipedema treatment:
Biomarker Research
Analysis of aspirate components may eventually allow surgeons to predict which patients will respond best to different surgical approaches, personalizing treatment plans based on individual tissue characteristics.
Technique Refinement
Better understanding of tissue properties is leading to improved surgical techniques that can more effectively address the unique challenges of lipedema tissue while minimizing complications.
Combined Therapies
Research into the biochemical abnormalities in lipedema tissue may lead to adjuvant treatments that can be combined with surgery to improve outcomes and reduce recurrence rates.
Making Informed Decisions
For patients considering lipedema reduction surgery in Missouri and the surrounding region, Dr. Wright’s expertise provides access to the most current understanding of these complex procedures. His commitment to evidence-based care means that treatment recommendations are based on scientific research rather than marketing promises or unrealistic volume claims.
The key to successful lipedema surgery lies in understanding that effective treatment addresses the underlying disease process, not just tissue volume. By focusing on pain relief, functional improvement, and quality of life enhancement, patients can achieve meaningful, lasting results that go far beyond what any volume measurement can capture.
Ready to learn more about evidence-based lipedema treatment that prioritizes your symptoms over arbitrary volume goals? Contact Dr. Wright’s office to schedule a comprehensive consultation. Our team understands the complexity of lipedema and is committed to helping you achieve realistic, meaningful improvements in your quality of life through personalized treatment planning.